Patient Education
Keratoconus
Keratoconus
Keratoconus (kerato=cornea; conus=cone-shaped) is a progressive disease of the cornea causing it to thin and change shape. This degenerative disease usually appears in the teens or early twenties, and is sporadic in the majority of cases. Only 10% of cases have a positive family history of keratoconus.
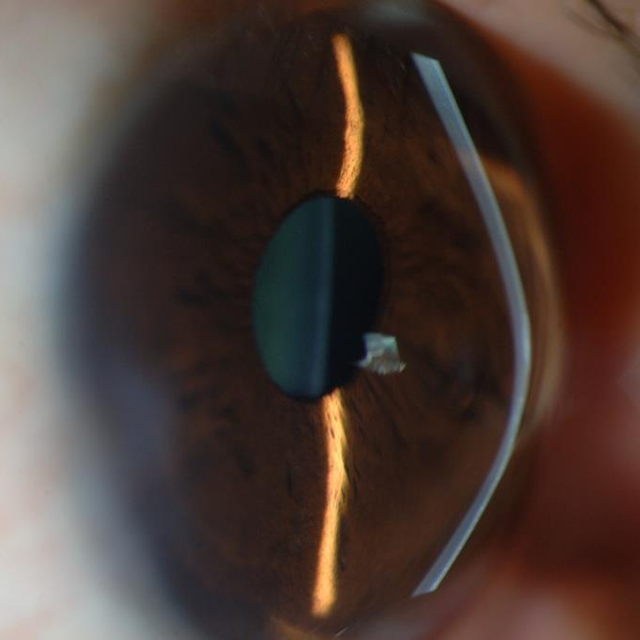
The cornea is normally round and spherical shaped, but with keratoconus the cornea becomes thinned and starts to bulge, thus distorting the cornea and resembling more of a cone shape. These changes affect the way light enters the eye, preventing the light from focusing precisely on the macula. As the disease progresses, the cone becomes more pronounced, causing further blurriness and distortion of vision. Because of the cornea's irregular shape, patients with keratoconus are usually very nearsighted and have a high degree of astigmatism.
- Symptoms
- Detection & Diagnosis
- Treatment
The typical patient with undiagnosed keratoconus complains of deteriorating vision at both distance and near, usually occurring in one eye first. There may also be complaints of glare, halos, ghosting of images, light sensitivity, and a general irritation of the eyes. For some, this advances over decades and may be very subtle, whereas with others it advances more quickly.
Diagnosis is only possible with routine eye examinations. The exam will include a measure of the corneal shape and steepness (using a keratometer and topographer), and the corneal thickness (using a pachymeter). A large amount or change in astigmatism is also characteristic of keratoconus. The doctor will also evaluate of the cornea, looking for signs such as scarring, corneal wrinkling, and shape changes.
Early/Mild keratoconus - glasses or soft contact lenses
Moderate keratoconus - rigid gas permeable (RGPs), hybrid, scleral, or semi-scleral contact lenses
Advanced keratoconus - Corneal surgery (penetrating keratoplasty)
In the early stages, eyeglasses or soft contact lenses often fully correct the refractive error. As the condition progresses glasses and soft contact lenses become inadequate at fully corrrecting the high astigmatism and nearsightedness. This occurs as the cornea becomes progressively steeper and distorted. When this happens, rigid gas permeable contact lenses (RGPs), hybrid contact lenses, scleral or semi-scleral lenses become the treatment of choice. There are a variety of specialty contact lenses designed specifically for keratoconic patients. These designs, as well as the optical tear layer that is created underneath the lens, results in optimal comfort and vision for the keratoconic patient.
Fitting keratoconic patients with contact lenses is difficult and time-consuming, so one can expect frequent follow-ups to fine-tune the fit and prescription. Furthermore, patients require frequent eye examinations as this conditin is progressive, and will cause further corneal thinning and distortion. Then the process will begin again, altering the contact lens fit and prescription for clear and comfortable vision.
If RGP contact lenses are not stable on the cornea, despite all other attempts, "piggybacking" may be an option. This is where a soft contact lens is worn on the cornea with an RGP lens on top. The soft contact lens is larger and can bend more easily to adhere to the shape of the distorted cornea, thus stabilizing the fit and minimizing the movement of the RGP lens on top.
There is also a procedure called corneal collagen cross-linking or CXL. In this procedure the outer layer of the cornea (called the epithelium) is removed to allow entry of riboflavin, a type of B vitamin, into the cornea, which then is activated with UV light. This strengthens the corneal tissue to halt or slow the progression of the bulging of the cornea in keratoconus.
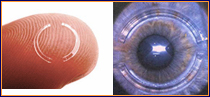 Intacts are another option where small plastic rings are inserted in the periphery of the cornea in an attempt to flatten the already steepend surface. This device received FDA approval in August 2004, and has shown to be effective in reducing nearsightedness and astigmatism in keratoconic patients where glasses and contact lenses no longer provide functional vision.
Intacts are another option where small plastic rings are inserted in the periphery of the cornea in an attempt to flatten the already steepend surface. This device received FDA approval in August 2004, and has shown to be effective in reducing nearsightedness and astigmatism in keratoconic patients where glasses and contact lenses no longer provide functional vision.
Lastly, when a keratoconic patient cannot achieve acceptable vision with glasses, intacs, or the cornea is unable to tolerate the fitting of a contact lens, or the cornea becomes scarred and obstructs vision, surgery becomes the final option. This surgery involves removing a full-thickness button of corneal tissue and replacing it with donor corneal tissue (ie. corneal transplant), and is called penetrating keratoplasty.
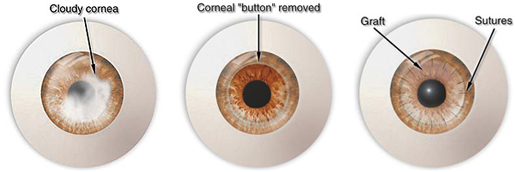
This is always the last option, as there are greater risks with this procedure. And, although there is a 95% success rate, 25-30% may require contact lenses after surgery.